In Clinical news
Bookmark
Record learning outcomes
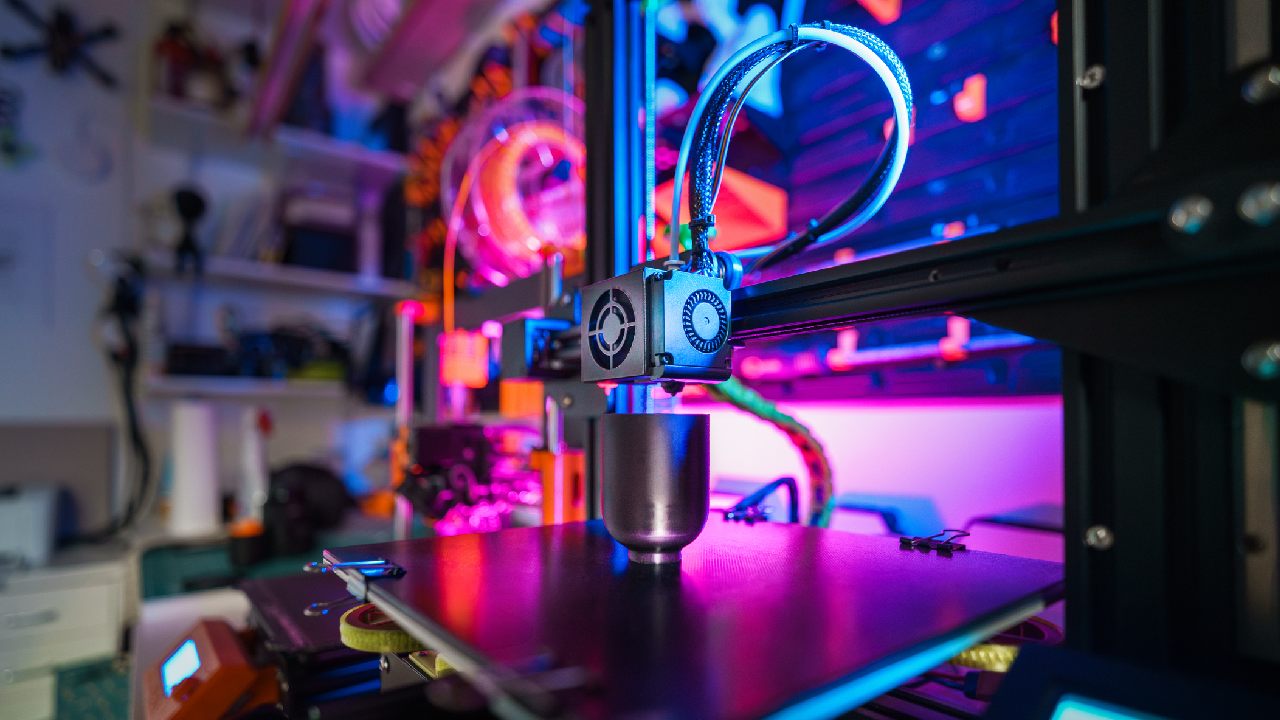
During the early 1980s, American engineer Charles Hull developed the first 3D printer, which deposited thin layers of an acrylic-based photopolymer onto a surface.
UV light simultaneously crosslinked the photopolymer creating a solid object.1 Today, 3D printing can be found in every aspect of prototype design and manufacture with some healthcare applications seeming to come directly from the pages of science fiction. For example, 3D printing can manufacture accurately fitting orthopaedic implants, prosthetics and dentistry products. Scaffolds can also precisely target medicines, such as delivering the antibiotic rifampicin for osteomyelitis (bone infection).1
Certain cells can adhere to the biomimetic scaffold, where they proliferate and differentiate. 3D ‘bioprinting’ can create, for example, cardiac and skeletal muscle, cartilage, ligaments, tendons and even entire organs, such as tracheal grafts.1
3D printing could also customise polypills. Michael Repka, professor of pharmaceutics and drug delivery at the University of Mississippi, notes that 3D printing can tailor medications’ size, shape, dosage and content to each patient. “Pharmaceutical companies have a one-size-fits-all approach to dosage, but that doesn’t work for everybody,” he says. “With [3D printing], we can tailor that dosage to what the patient needs.”
Different geometries
In 2019, a team from China 3D-printed polyvinyl alcohol tablets containing paracetamol. The researchers embedded three different geometries (‘cylinder’, ‘horn’ and ‘reversed horn’) in the same tablet. Each geometry demonstrated different release profiles so researchers could tailor the release characteristics according to the patient’s needs. For example, the cylinder’s constant release rate keeps blood levels within a specific range. The horn results in a gradually increasing concentration, which may help overcome drug resistance. The reversed horn shows a gradually decreasing profile.2
More recently, researchers from the University of Nottingham’s Centre for Additive Manufacturing customised pharmaceutical tablets with tailored drug release profiles. The study showed that 3D printing can create tablets combining dissimilar materials, such as combining water soluble and insoluble drugs. The system can print 56 pills in a batch.3
The researchers used Multi-Material InkJet 3D Printing to manufacture tablets using a water-soluble, UV-cured carrier (poly-4-acryloylmorpholine). The tablet’s interior structure released aspirin at a range of rates including slow (0.98mg/min), fast (4.07mg/min) and multi-stepped (2.17 then 0.70mg/min) dissolution curves. The authors say that the system offers “realistic opportunities for advanced pharmaceutics manufacturing and personalised medicines”.3
“The future of prescribed medication lies in a personalised approach,” says study author Professor Felicity Rose, from the University of Nottingham’s school of pharmacy.
“Up to half of people in the UK don’t take their medicines correctly and this has an impact on poorer health outcomes with conditions not being controlled or properly treated. A single pill approach would simplify taking multiple medications at different times and this research is an exciting step towards that,” she says.
Size matters
Michael Repka and colleagues contributed a chapter to a new book, 3D Printing: Emerging Technologies and Functionality of Polymeric Excipients in Drug Product Development.4
“There are many limitations with conventional medications, like the size of the tablet or capsule,” adds Dr Dinesh Nyavanandi from the University of Mississippi, and chapter co-author. “For paediatric and geriatric patients, the size of the tablet is a big challenge. Many of the paediatric and geriatric population will skip their medication because of tablet size.”
3D printing could be used to manufacture smaller doses and customise a medicine’s colour or shape, including creating a familiar shape, such as a gummy bear, to encourage young children to take their medicine.
“For every medication, stability and storage are the most common challenges,” adds Dr Sagar Narala, also from the University of Mississippi. “If we use 3D printing [the medication] is made when it is needed in a pharmacy setting, and we can avoid stability or storage issues. 3D printing can avoid large-scale manufacturing, [which is] particularly beneficial for drugs with limited markets.”
Despite the considerable potential, it’ll be some time before community pharmacists are using 3D printing to pimp their patients’ pills. Michael Repka notes that 3D printing is currently “too slow and costly for widespread use”. Nevertheless, if researchers can speed up the process and cut the costs, pharmacists of the future could find themselves printing medication on an as-needed basis.
References
1. Scientific Reports 2020; 10:14023
2. Scientific Reports 2019; 9:12487
3. Materials Today Advances 2024; 22:100493
4. See link.springer.com/book/10.1007/978-3-031-46015-9